Global Initiatives on AMR (Antimicrobial Resistance): What It Means for Pharma Pipelines and Future Markets?
In-depth market intelligence to support growth and planning.
The phenomenon of antimicrobial resistance (AMR) poses a significant threat to human health. It has been weakening the effectiveness of medicine over the past few years, posing a serious challenge to both human and animal healthcare systems. To acknowledge the multidimensional, cross-sectoral character of AMR, global policies such as the World Health Organization's Global Action Plan on AMR, the Global Antimicrobial Resistance and Use Surveillance System (GLASS), the Quadripartite Alliance (WHO, FAO, WOAH, UNEP), and the European Partnership for One Health AMR are recommending coordinated international engagements. These initiatives attempt to implement a “One Health” approach to spur innovation, coordinate monitoring and enhance stewardship across sectors, as well as curb the rise in resistance.
For the pharma industry, AMR is simultaneously a threat and a single-shot opportunity. Foregoing incentives to discover new antibiotics has fallen short due to short treatment courses, lack of profitability and advanced generic competition, which has pushed all but the most prominent players out of the market. However, evolving global regulations, collaborations and economic priorities are reshaping industry fundamentals, financial models, regulatory frameworks, and cooperative systems.
Such radical changes are prompting major pharmaceutical companies to reassess their plans, diversify their product range, and partner with companies that have a strong environmental business record. The use of bacteria that can resist drugs is the most probable cause for pharmaceutical companies to reconsider their engagement with the global healthcare ecosystem and outline future innovations.
Global AMR Initiatives
Antimicrobial resistance (AMR), which is a significant concern for global health, is a case that calls for teamwork, not only among various sectors but also across borders. Apart from a long list of programs aimed at advancing surveillance, accelerating research, improving diagnosis and promoting the appropriate use of antibiotics, governments, global organizations and associations have also been implementing these ideas. Indeed, such initiatives are One Health-centric, a notion that identifies the links/connectivity/responsiveness between human, animal and environmental health. Below is a summary table of a few landmark initiatives that are reshaping the global response.
Table: Overview of Leading AMR Initiatives
|
Initiative |
Organization |
Description |
|
Global Action Plan on Antimicrobial Resistance |
World
Health Organization (WHO) |
The
World Health Organization's (WHO) Global Action Plan on Antimicrobial
Resistance (AMR) provides a roadmap for combating the emergence and spread of
AMR, which poses substantial threats to global health, food security and
socioeconomic development. The plan underlines the importance of coordinated
actions across sectors to combat the misuse and overuse of antimicrobials in
human medicine and agriculture. |
|
Global Antimicrobial Resistance
and Use Surveillance System (GLASS) |
World Health Organization (WHO) |
The World Health Organization launched the
Global Antimicrobial Resistance and Surveillance System (GLASS) in 2015 to
enhance surveillance of antimicrobial resistance (AMR) and inform preventive
measures against it. The system includes a dashboard that displays worldwide
antimicrobial usage (AMU) and resistance data in interactive visualizations,
allowing users to access detailed data from participating countries. |
|
European Partnership on One Health AMR (OHAMR) |
European
Commission and EU Member States |
The
European Partnership on One Health Antimicrobial Resistance (EUP OHAMR)
brings together 53 organizations from 30 countries in the EU and beyond to
address antimicrobial resistance (AMR) concerns from various sectors and
viewpoints. The alliance adopts an integrated One Health approach,
recognizing that human, animal and plant health are interrelated and closely linked
to the environment. |
|
Global collaboration to tackle
antimicrobial resistance |
The Fleming Initiative, GARDP and FIND |
A recently established global program aims to
combat antimicrobial resistance by enhancing diagnostic technologies,
enabling physicians to detect illnesses more quickly, optimizing antibiotic
use, and reducing resistance. This will ensure long-term access to viable
therapies for populations worldwide. |
Source: Official Website of Organizations
These initiatives represent a coordinated global response aimed at addressing the complex issue of antimicrobial resistance. They aim to enhance monitoring, research, diagnosis and stewardship, while increasing awareness by incorporating the One Health concept across various sectors. Moreover, thorough cooperation, effective resource allocation and creative thinking are essential to foster effective action and sustain the effectiveness of antimicrobials in the future. These undertakings underscore a fundamental shift in the AMR market, driven not only by demand but also by policy regimes, public-private partnerships and innovative financing models.
What does this mean for Pharma Pipelines?
The fight against antimicrobial resistance (AMR) is profoundly changing the pharmaceutical sector. For a long time, new antimicrobial supplies were scarce and underfunded. Now, the involvement of both the public and private sectors, new funding sources and the use of innovative technologies are reviving it. However, most of the problems in this field are still connected with the stage of moving the agents into advanced trials. The sector, however, is showing renewed diversification and interaction.
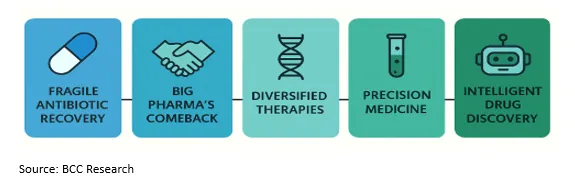
Fragile Antibiotic Recovery: For a long time, the process of discovering new types of antibiotics has remained largely unchanged and the pace has been quite slow. Most discoveries originate from small and medium-sized biotechnological firms rather than large pharmaceutical companies. These innovators often encounter significant financial challenges when they must maintain their late-stage clinical programs, necessitating the availability of new funding and incentive frameworks to support them.
Big Pharma's Reluctant Comeback: Pharma giants have already worked through and executed their next moves to regain the driver's seat ahead of antimicrobial resistance, but their carefully planned strategy, which includes selective collaborations and licensing deals rather than a comprehensive internal R&D approach, remains in place. In April 2025, Shionogi and Link Healthcare signed a licensing agreement that will grant the latter full marketing rights for cefiderocol in Australia and New Zealand, exemplifying how collaborations can be leveraged to access the benefits of risk mitigation, overcoming supply barriers and revitalizing the antibiotic supply.
Beyond Antibiotics: A Diversified Approach—New AMR solutions are not limited to the use of traditional antibiotics. In addition to antibiotics, bacteriophages, antimicrobial peptides, microbiome therapies, vaccines, and rapid diagnostics are all being introduced and are the future of a multi-modal therapeutic ecosystem. Such diversification not only deepens the scope of therapy but also has a positive effect on resisting the development of resistance.
Precision Integration and Emerging Technologies: Pharma R&D is increasingly aligning with precision medicine. The development of companion diagnostics is becoming increasingly standard in pharmaceutical pipelines, enabling the responsible use of antimicrobials. At the same time, AI drug discovery and CRISPR, which is used for gene editing in antibiosis targets and synthetic biology, are completely reshaping upstream research by allowing for the rapid identification of novel compounds and engaging trial participants, making them more likely to succeed.
Contemporary AMR policies are developing new approaches to funding and scaling innovations. Subscription-based models, such as the UK NHS Pilot (2024) and the US PASTEUR Act, serve as benchmarks for innovative systems that pay for the value of antibiotics rather than the quantity, thereby encouraging the sustainability of stewardship programs while maintaining commercial viability. Brave programs, such as CARB-X, the Global AMR Innovation Fund (GAMRIF) and the EU Innovative Health Initiative (IHI), provide substantial funding and offer the necessary guidance to developers of early-stage products.
Additionally, strategic alliances such as Pfizer's partnership with GARDP and Roche's collaboration in the field of rapid diagnostic technologies are enhancing simultaneous access and facilitating development. These movements are a clear indication of a departure from isolated R&D towards a concerted, multi-actor model that is concerned with planet-wide resilience and the sustainable use of antibiotics.
The Market Outlook: Challenges and Opportunities
Fragile Demand Dynamics: Unlike most therapeutic segments, the AMR market is not inherently demand-driven. Stewardship strategies intentionally constrain antibiotic utilization to ensure efficacy, and in doing so, constrain sales volume. This prevents big-pharma companies from amortizing substantial R&D expenditures, building a fragile and unsustainable business model.
Financing Gaps: Most new antibiotics are developed by small and medium-sized biotech enterprises. Unfortunately, these enterprises lack sufficient financial resources to complete the late-stage clinical trials of their drugs, which are typically lengthy, risky, and expensive. Without a stronger financing regime or alliances, many promising medicines never reach the market.
Regional Disparities: A notable feature of antibiotic resistance in low- and middle-income countries (LMICs) is the poor health infrastructure prevalent in these regions. Poor monitoring systems, incorrect diagnostics and the limited availability of high-quality medicines are factors that make these areas more susceptible to the uneven landscape, which is more resistant to coordinated global efforts in fighting AMR.
Key Opportunities
Policy-Driven Growth: AMR stands out because its market potential is largely driven by enabling policies, rather than raw demand. Pull incentives, subscription-based pay plans like the UK's "Netflix model," and guaranteed procurement programs can de-risk investments. These drivers have the capability of propelling AMR into a thriving market from a stagnant business area.
Diagnostics and Stewardship Platforms: The future of AMR is not solely reliant on novel antibiotics but also on rapid diagnostics and stewardship solutions. These solutions allow doctors to administer the proper medication at the appropriate time and help existing antibiotics last longer. Diagnostics and stewardship platforms would create substantial and sustainable revenue streams, even exceeding drug sales.
Next-Gen Innovation: Advanced technologies have become the gateway to a diverse range of new possibilities for Antimicrobial Resistance (AMR) solutions. Originating from the realm of artificial intelligence, compound screening is a primary accelerator for discovery timelines, while CRISPR antimicrobials offer more precise, targeted strategies and microbiome treatments unveil a whole new, novel preventive field. While vaccines represent a strong means to diminish infection rates, they collectively diversify the therapeutic arsenal and unveil new growth opportunities.
Future Outlook: Pharma’s Emerging Opportunity
The future of antimicrobial resistance (AMR) must be considered with caution, but there is still room for optimism. As AMR continues to escalate, it will endanger the entire global healthcare system, as well as various economies. Simultaneously, the introduction of fresh incentives and collaborative funding models, coupled with groundbreaking scientific breakthroughs, appears to reinvigorate the antibiotic pipeline. Companies that invest in the development of innovative and novel antimicrobial resistance (AMR) vaccines, as well as in the management of AMR, will be the winners. They will be the first to meet the huge market demand for affordable and highly effective antibiotics. The debut of AMR highlights the need for adaptable, robust, intelligent and far-sighted pharmaceutical responses to the well-being of the earth's future population.
Conclusion
AMR is a slow-moving pandemic, but unlike many others, the world has the foresight and capabilities to react. Initiatives worldwide have laid the groundwork for a new AMR market space where science, policy, and pharma intersect.
For pharmaceutical organizations, this is a compliance imperative, it is an opportunity to lead. By adopting new business models, making investments in diversified solutions and engaging with global stewardship objectives, the pharmaceutical industry can turn AMR from a potential catastrophe into a 21st-century defining opportunity.
Looking for Consulting & Advisory Projects
