Robotic Process Automation in Healthcare Claims Management
AI-Driven RPA Solutions for Streamlined Healthcare Claims
The healthcare claims management landscape is rapidly evolving with the widespread adoption of robotic process automation (RPA). This rapid growth reflects the industry's increasing need for efficiency, accuracy and cost-effectiveness to meet the complexity of claims processing. The growing administrative burden, combined with rising costs and changing regulatory requirements, makes digitalization and automation of workflows look more like a necessity than an option. On the other hand, the combination of AI technology with RPA is broadening the scope of automation to handle complex and unstructured data with more adaptability. For healthcare executives and operational leaders, the decision to implement RPA is no longer just about system improvement but about a strategic move required to remain operationally competitive and keep pace with the fast-changing landscape of healthcare patient outcomes.
The Impact of RPA Technology in Healthcare Claims
Healthcare
claims have numerous complexities and various steps, which include evaluating
clinical data, verifying insurance coverage, deciphering medical codes,
ensuring compliance and coordinating benefits among multiple parties. If these
steps were to rely on outdated and manual systems, inefficiencies would quickly
escalate to include unprocessed claims, delayed reimbursements, compliance
risks, and costly audits.
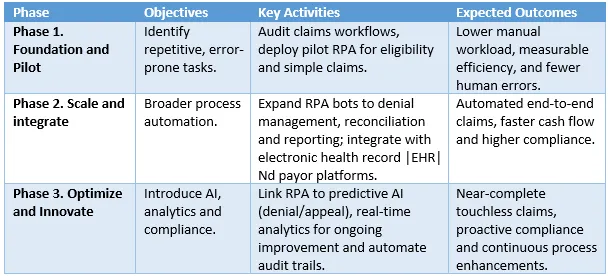
By the end of 2026, organizations that execute this roadmap may see shorter claim cycles, lower costs and stronger compliance, serving as a context-specific reference model.
Since 2023, many organizations have reported automating a large share of repetitive claims steps; exact coverage varies by workflow and payer rules, which include the following:
- The integration with external databases for eligibility verification.
- Pre-authorization activities before treatment are confirmed.
- Automated data entry to reduce transcription errors.
- Rule-based claim adjudication for both the issuing of balances and denials.
- Payment posting and reconciliation.
- Digital audit and compliance reporting.
The latest developments suggest that AI, NLP and cognitive automation collectively contribute to the advancement of healthcare RPA. The COVID-19 pandemic has been a decisive factor in this respect, as it has accelerated the digital transformation, likely due to the urgent need for remote work and other digital solutions that relate to patients and their data.
Key Advantages Driving RPA Adoption
1. Operational
Efficiency and Cost Reduction
By handling claims repetitively with reduced
human interaction, robotic process automation (RPA) reduces manual effort. It
shortens the time taken, as well as the portion of the cost attributable to
rework caused by human errors. For example, Massachusetts Health demonstrated
that RPA could be the solution for expediting Medicaid claims without the need for
a human workforce for reimbursements.
2. Accuracy
and Compliance
Healthcare billing codes, item rules and
regulations are constantly changing. These RPA bots, which strictly adhere to
the set of rules, significantly minimize errors caused by human negligence;
thus, compliance is also improved. To become even more transparent for
regulators and payers, these bots may provide generated audit-ready logs.
3. Workforce
Productivity and Satisfaction
One of the leading reasons for healthcare
worker burnout is the repetitive performance of administrative tasks. Through
the automation of such tasks, RPA enables healthcare professionals to focus on
patient engagement, exception handling and process optimization, ultimately
leading to high job satisfaction and staff retention.
4. Faster
Turnaround and Improved Patient Experience
Systems with automation speed up claims
processing, allowing payments to be made faster and reducing denial rates to
near zero. At the same time, it ensures that administrative work is cut down
for the patient, resulting in an overall better patient experience.
5. Scalability and Flexibility
RPA platforms can easily scale to handle
fluctuating claim volumes without proportional increases in staff or
infrastructure. These can also adapt to new payer rules, coding changes, or
pandemic-driven reimbursement policies, ensuring business agility.
Recent Developments: AI + RPA Integration
While RPA alone automates rule-based tasks, integrating it with AI and Machine Learning (ML) introduces cognitive capabilities. This next generation of RPA, often called Cognitive RPA, allows bots to:
- Interpret unstructured data, such as physician notes or lab results.
- Analyze appeals and medical documentation using NLP.
- Handle complex claims that traditionally required human intervention.
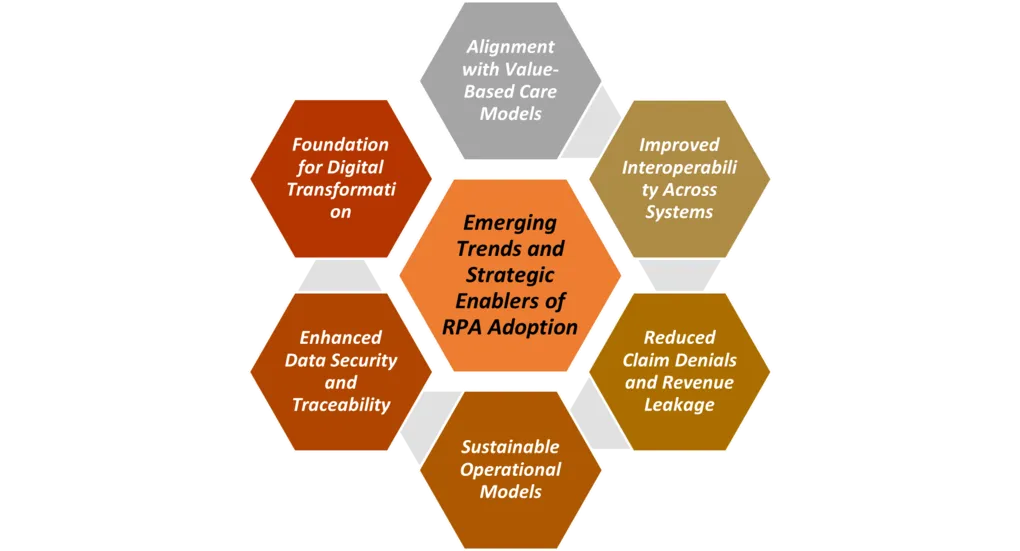
The healthcare industry is implementing RPA through the use of intelligent automation systems linked to Electronic Health Records (EHRs), Customer Relationship Management (CRM) systems and revenue cycle management software. This results in a smooth data flow and real-time tracking of the entire claims lifecycle. Advanced dashboards with analytics further enhance the functionalities of performance monitoring, bottleneck identification and continual process improvement.
Challenges and Considerations
Although RPA offers benefits, its implementation faces obstacles. The key challenges are:
- Identifying the right processes suitable for automation.
- Designing bots to handle exceptions effectively.
- Integrating with legacy systems.
- Ensuring data security and compliance with HIPAA and other regulations.
- Managing organizational change to align staff and stakeholders.
To succeed, healthcare providers must collaborate closely with vendors and ensure that implementations are scalable, secure and outcome driven.
Conclusion
RPA is a significant advancement in healthcare claims management. With RPA, healthcare organizations can reduce administrative overhead, decrease errors, accelerate the reimbursement process, and enable staff to focus on more creative tasks with the assistance of technology.
Moreover, when considering the combination of RPA and AI, it is not only about efficiency but also about intelligent, adaptable automation that supports sustainable innovation in healthcare. A healthcare leader who wants to remain competitive while delivering high-quality patient care should start with high-volume, rules-based steps and expand as governance and exception handling mature.
Looking for Consulting & Advisory Projects
